Priapism is defined as a persistent and painful penile erection.
What differentiates priapism from a normal erection, is that it is entirely unrelated to sexual arousal.
Priapism results in an erection that lasts for longer than four hours [1]. Priapism frequently occurs in men between the age of 40 and 50 years old.
In the United States alone, there are 8,000 visits to the emergency department each year because of priapism [2].
Most cases of priapism are due to alcohol or drug abuse (21%), trauma (12%), and sickle cell disease (11%) [3]. Left untreated, priapism can lead to long-term erectile dysfunction.
Sickle cell disease particularly increases one’s risk for developing priapism.
The chance of developing priapism in sickle cell patients is as high as 42%, and the rate of subsequent erectile dysfunction after an episode is 30%.
The most common complication of priapism is erectile dysfunction, which can occur in as many as 60% of cases [4].
However, recovery of the penile erectile function is seen in about 45% of patients who have sustained erections lasting from 24 to 36 hours [5].
In this article, we review the clinical presentation of priapism. We go through the signs and symptoms of priapism and discuss the management of this dangerous condition.
Causes of Priapism
Priapism is an uncommon condition, but it has been shown to affect up to 5 per 100,000 men annually. There are three main types of priapism. These are:
i) Ischaemic Priapism (low flow)
ii) Non-ischaemic Priapism (high flow)
iii) Stuttering Priapism (recurrent)
Ischaemic priapism is the most common type of priapism. It is the result of an impeded venous outflow from the spongy tissues of the penis. Ischaemic priapism accounts for the vast majority (95%) of cases.
These spongy tissues are termed as the corpora cavernosa. The occluded venous outflow prevents oxygenated blood from flowing into the corpora cavernosa.
This results in tissue ischemia (lack of oxygen). The muscles of the penis die and form scar tissue in a process known as fibrosis [6]. Several disease states and medications can cause Ischaemic priapism. These include:
- Cancer
- Spinal Cord Injury
- Sickle Cell Disease
- Glucose-6-Phosphate Deficiency
- Viagra
- Amphetamines
- Trazadone
- Cocaine
- Selective serotonin reuptake inhibitors (SSRIs)
Of the causes listed above, an overdose of Viagra in the treatment of erectile dysfunction is the most common cause.
Non-ischaemic priapism is usually caused by trauma to the penis. After perineal trauma, an abnormal connection forms between the penile arteries and the corpus cavernosum. This leads to an unregulated arterial inflow of blood into the spongy tissues of the penis, causing a persistent erection. This abnormal connection is termed as a fistula.
Stuttering priapism is defined as periodic episodes of prolonged erections. These episodes usually occur during sleep, or even with sexual stimulation, but tend to resolve spontaneously. Stuttering priapism tends to affect sickle cell patients more often than non-sickle cell patients.
Signs and Symptoms of Priapism
Priapism is usually painless in the majority of cases. Pain is generally present in ischaemic priapism, whereas it is absent in non-ischaemic priapism. In ischaemic priapism, there is a remarkable rigidity of the penile spongy tissues.
Diagnosis of Priapism
- Blood gas analysis: A cavernous blood gas analysis is usually done to confirm the diagnosis of ischaemic priapism. Ischaemic priapism accounts for 95% of all priapism cases. This procedure involves a needle extraction of penile blood, followed by a review of the gases within it.
In ischaemic priapism, there is a higher concentration of carbon dioxide and a lower concentration of oxygen within the penile blood. This is because of the venous inflow into the spongy tissues of the penis.
The pH of the venous blood is also likely to be less than 7.0. The cavernous blood gas analysis is, therefore, extremely useful in distinguishing between ischaemic and non-ischaemic priapism.
- Hemoglobin analysis: Because sickle cell disease accounts for 11% of all cases of priapism, a full blood count and hemoglobin analysis are also performed. This enables the identification of sickle cells, thereby confirming a diagnosis of sickle cell anemia.
- Radiological imaging: Radiological imaging can also be useful in the diagnosis of priapism. Doppler ultrasound is used to assess the blood flow within the penile arteries that supply its spongy tissues.
Impaired blood flow during ischaemic priapism can be detected with this imaging modality. In non-ischaemic priapism, the Doppler ultrasound will reveal an extremely high-velocity flow within the corpus cavernous. It can even detect the fistula between the penile artery and the corpus cavernosa that is responsible for this arterial inflow.
Management of Priapism
Because priapism is a urologic emergency that can lead to permanent erectile dysfunction, it is essential to diagnose and manage it in a timely fashion.
The overall goal is to reverse the persistent erection while maintaining the ability of erections in the future. The first step of management is to distinguish between ischaemic and non-ischaemic priapism. To facilitate this, a cavernous blood gas and Doppler ultrasound will be performed.
Ischaemic priapism is an emergency because if left untreated, the penile muscles die in a process known as necrosis.
Non-ischaemic priapism, on the other hand, is not an emergency, as the penile tissues are still well oxygenated. We shall discuss the management principles of ischaemic and non-ischaemic priapism separately.
Ischaemic priapism
Aspiration: The first-line intervention for ischaemic priapism is an aspiration of the cavernous blood [6]. This is a painful procedure. It involves the insertion of a sterile catheter into the cavernous space to relieve it of the venous blood.
The catheter is inserted at the lateral aspect of the penile shaft. The lateral approach is preferred, as it avoids damaging the urethra (urinary tube) and the nerves which supply the penis. A syringe is attached to the catheter. This allows for the evacuation of blood from the corpora cavernosa. The cavernous space is simultaneously irrigated with saline.
Sympathomimetic agents: Some physicians may also administer sympathomimetic agents into the cavernous space. Sympathomimetic agents are drugs such as phenylephrine and ephedrine. The addition of these sympathomimetic agents has been shown to result in a higher resolution of ischaemic priapism [1].
Furthermore, the risk of post-priapism erectile dysfunction is reduced with this approach.
Surgical shunting: For ischaemic priapism that has gone on for more than 48 hours, it can be very challenging to resolve. In these cases, physicians opt for a more invasive course of treatment for priapism.
Surgical shunting is the management option of choice in these cases. The goal of a surgical shunt procedure is to create an artificial connection between the corpora cavernosa and a distant site. This allows the trapped venous blood to be relieved and extracted. Various types of shunts can be used in this approach. These shunts are displayed in Figure 1 below.
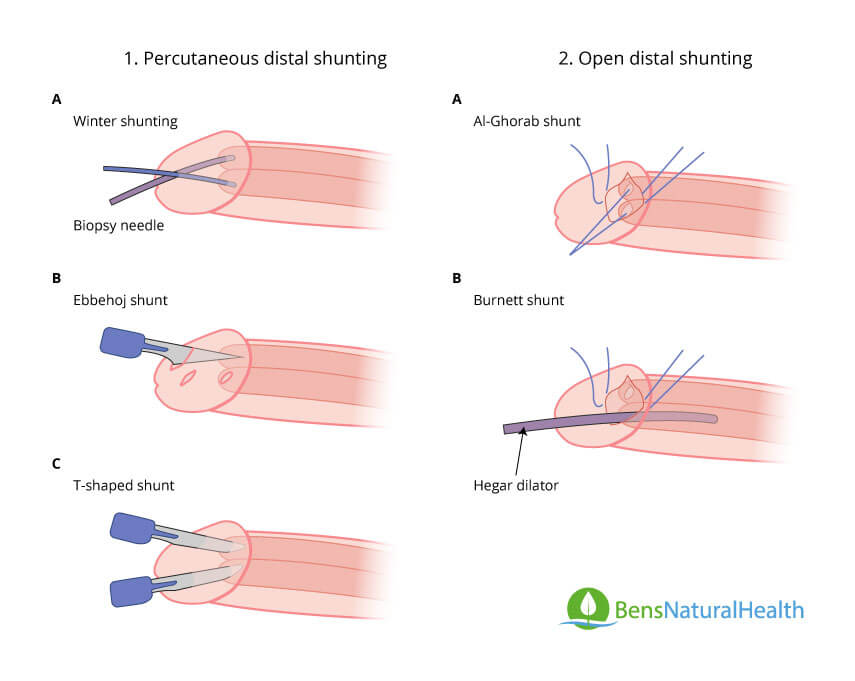
Although these shunts appear to be dramatic, painful, and radical, they are necessary to prevent long-term erectile dysfunction.
These shunts are a last resort that is typically considered only for the treatment of priapism that has lasted for longer than 48 hours. Keep in mind that these shunts constitute a surgery. Hence, patients will be sedated for the duration of the procedure, making it painless.
After the trapped venous blood is excavated, the shunts are closed. Of the shunt approaches shown above, the Winter and Ebbehoj shunt approaches are preferred nowadays as they are generally minimally invasive.
Penile Prosthesis: One alternative to the creation of a shunt in the prolonged case of ischaemic priapism is a penile prosthesis. Urgent penile prosthesis implantation is advocated as an alternative initial management strategy by urologists.
The implantation of a penile prosthesis reduces the recurrence of painful priapism for the patient [7].
Non-ischemic priapism
Nonischemic priapism often goes away without treatment. As there is a low risk of damage to the penis, your doctor might suggest a watch-and-wait approach. Methods such as putting ice packs and pressure on the perineum may help end the erection.
In some cases, surgery might be necessary. Treatment such as an absorbable gel, that temporarily blocks blood flow to your penis may be administered.
Supplements for Priapism
Supplements can be beneficial for patients who have suffered priapism, or who are looking to prevent an episode of priapism. After all, ischaemic priapism can be painful and lead to long-term erectile dysfunction. This is an even more significant concern for men with sickle cell disease.
It must be noted that oral supplements cannot treat an active case of priapism.
We strongly advise all our readers to present to the emergency department urgently if they have a prolonged and persistent erection that is unrelated to sexual arousal.
Keeping in mind that one of the most common causes of priapism is an overdose or dependence on Viagra, supplements that naturally increase the blood flow in the penis can prevent priapism. Naturally occurring compounds are preferable to drugs for a few reasons.
First, they are without adverse effects and are safe for consumption. Second, they cost a lot less than drugs, which are heavily marked up by pharmaceutical companies. Third, they have systemic benefits that enhance overall health (and not just erectile function).
There are a plethora of supplements that can increase erectile function naturally.
- Ginseng: Of these, ginseng has been heavily studied. One systematic review in 2018 evaluated 24 randomized controlled trials and found that ginseng is an effective herbal treatment for erectile dysfunction [8]. At Ben’s Natural Health, ginseng has been an indispensable ingredient in our Male Boost tincture. Ginseng is also conferred neuroprotective, anti-inflammatory, anti-oxidant, and anti-microbial benefits to the body [9].
- Arginine: Another systematic review and meta-analysis, which evaluated 10 randomized controlled trials, found that arginine supplements result in an improvement in mild to moderate erectile dysfunction [10].
- L-citrulline: A study in 2011 found that oral L-citrulline supplementation improved erectile hardness in men with mild erectile dysfunction [11]. L-citrulline is a non-essential amino acid that is converted into L-arginine by the kidneys. This explains why L-arginine is also beneficial for erectile health.
- Vitamin D: Concerning priapism itself, Vitamin D is a vital supplement for the following reasons. First, men with sickle cell disease have increased catabolism and deficits in energy. This leads to nutritional deficiencies, including Vitamin D deficiency. Vitamin D is essential for calcium homeostasis and bone mineralization.
Vitamin D deficiency has been observed to lead to sexual dysfunction in healthy men [13]. Supplementation has also been found to treat and reduce the rates of erectile dysfunction in men with Vitamin D deficiency [14]. Indeed, one systematic review and meta-analysis concurred with these findings [15].
At Ben’s Natural Health, we have written another article emphasizing the importance of Vitamin D for overall health. Furthermore, we have formulated our proprietary blend of naturally occurring compounds.
Ben’s Total Health for the Prostate contains a whopping 5000 IU (125mcg) of Vitamin D. This is between 5 to 10 times the amount of Vitamin D3 found in products by leading multivitamin companies.
Conclusion
The management goals of ischaemic priapism are to relieve the cavernous space of trapped venous blood. This is achieved through aspiration, irrigation, and the administration of sympathomimetic drugs.
Supplements such as ginseng, L-citrulline, L-arginine, and Vitamin D are extremely useful in preventing priapism as well as recurrence. This is because the most common cause of ischaemic priapism after sickle cell disease is the overdose of or dependence on Viagra.