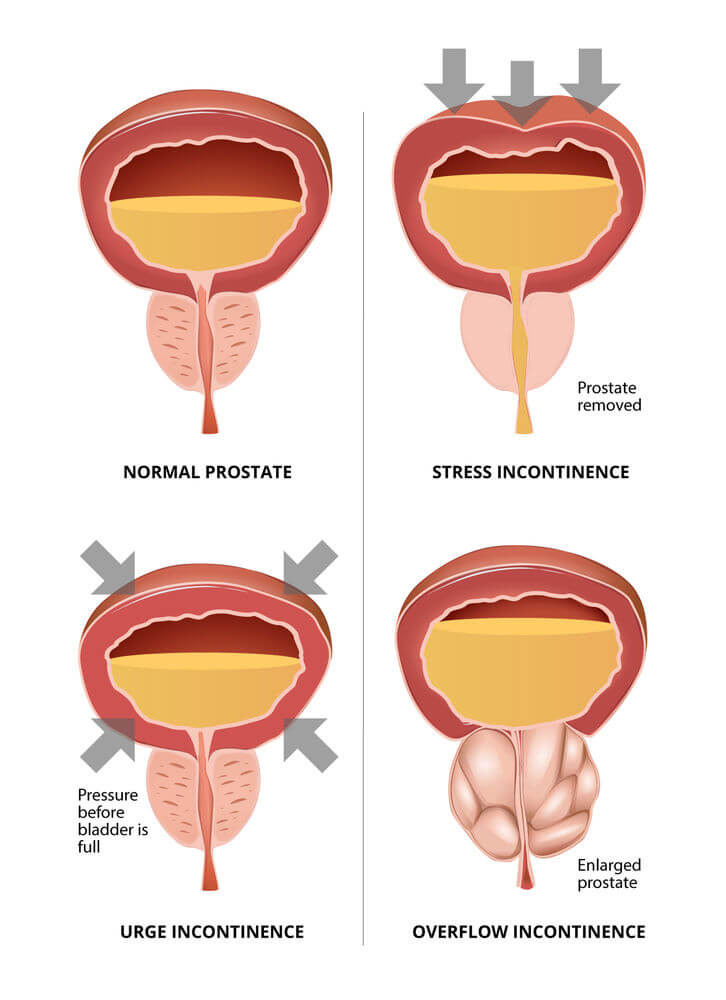
Incontinence refers to the inability to control the release of urine. It is a typical side effect of a radical prostatectomy and other prostate surgeries. The prostate surrounds the urethra and is in close proximity to the urinary bladder.
Prostate removal can lead to potential damage to the nerves and muscles surrounding the bladder and urethra. This damage often results in urinary incontinence as well as impotence.
The reported statistics on the likelihood of developing incontinence after a radical prostatectomy vary considerably. The literature reviewed cites levels from about 2 to 15 percent.
Some men with initial post-surgery incontinence will regain bladder control with time; others may not. If control is spontaneously regained, It will usually be in less that one year. n this article, we will explore the impact of urinary incontinence and available treatment options.
Get Your FREE PSA Lowering Diet Plan!
- Naturally lower PSA levels
- Reduce nighttime trips to the bathroom
- Enjoy better bladder control and urine flow
Statistics on Incontinence After Surgery
A large number of men experience incontinence after a total prostatectomy, at least temporarily. For some lucky few, the incontinence will end in a short time, others will suffer for a few months, and some may live with it permanently.
Some doctors may focus more on the patients with fewer problems, possibly overlooking those with persistent issues.
Generally, a Foley catheter is inserted during or just before the surgery to take care of temporary incontinence caused by the surgery. This device will be left in the patient for about a week after surgery.
A Foley catheter is a flexible tube that is passed through the penis and into the bladder to drain urine. It is held in place in the bladder by a small balloon inflated at insertion time. Its other end connects to a collection bag. It is an indwelling urinary catheter designed for short-term use.
On a follow-up visit after surgery, the surgeon will remove the Foley catheter, and the man can attempt natural voiding. In many cases, natural voiding is unsuccessful, and the catheter is left in for another cycle. Usually, the patient is introduced to absorbent pads as a temporary measure until natural voiding is successful.
- According to studies, for certain surgical procedures, up to 40 percent of men may experience temporary urinary issues, such as wearing protective pads or experiencing urinary leakage, one year after surgery.”
These revisions aim to make the content more compliant with CAP and ASA codes by avoiding sweeping claims about medical professionals and providing context and clarity when discussing statistics related to medical outcomes. A study of 901 men treated with surgery, published in the Journal of the National Cancer Institute, found that 14 to 16 percent were incontinent five years after treatment. [ Potosky ]
Levels of Incontinence
While incontinence is an inevitable side effect of prostate surgery, its severity can also vary considerably. Some men can experience total incontinence, whereby they have no control over their urinary sphincter, and urine simply drains as it is produced by the kidneys. This is usually the case immediately after surgery until the trauma to the surrounding nerves calms down.
On the other hand, some men achieve a degree of continence relatively quickly, with the exception of relatively minor leakage. Others find themselves left with stress incontinence, whereby a sneeze, laughter, or cough causes a significant amount of urine to be released. Others find themselves totally incontinent.
To remain socially active, these men have only one immediate choice, the absorbent pad or diaper. Pads today are made in many sizes. While wearing one can be quite discrete, it is still a major disruption to a man′s quality of life.
If incontinence persists beyond a year, other treatment options may be considered, including surgical ones, each with its own set of potential side effects. While there are limited options for addressing incontinence, both surgical and non-surgical, it’s important to note that none can fully replicate the function of a healthy body.
Kegel Exercises May Help
Kegel exercises or pelvic floor muscle training) exercises have been shown to help with incontinence. They target and strengthen the pelvic floor muscles. While incontinence caused by surgery is not a matter of weakness of these muscles, strengthening them may assist in urinary control.
The prostate gland can be found under the bladder, surrounding the urethra. The urethra is a tube that carries urine through the penis out of the body.
However, during prostate treatment, the muscles surrounding the prostate can become gradually weakened, resulting in urine leakage and even incontinence.
A Kegel exercise starts as if you are trying to urinate and then holding it by tightening the muscles that control urine flow. As urine flow starts, tightening the muscles will stop it. The muscles that control the urine flow are the pelvic floor muscles and those you need to strengthen.
Pelvic floor muscle exercise is done by tightening and relaxing this set of muscles at least three times per day. Each set consists of tightening and holding for a period of 3 to 5 seconds and repeating about 10 times several times per day. There are many Internet websites with instructions on implementing various Kegel exercises.
For many men locating the pelvic muscles can be a struggle. To find your pelvic muscle try to stop and start your urine stream when urinating.
Remember not to tense your buttocks or your legs and abdomen. Also, take note to keep breathing calmly.
When you have successfully slowed down or stopped your urine, you will be able to hit the target muscle. The muscles you use to stop your urine flow are your pelvic muscles, and these are the ones you want to strengthen.
When incontinence is due to surgical trauma, whether or not it can be resolved with Kegal exercises depends, and the amount of damage sustained by the surrounding nerves. For surgically induced incontinence, it may take 4 to 6 weeks to see significant improvement. If no improvement is noted in 4 to 6 weeks, talk to your doctor about other options.
Biofeedback
Biofeedback is a mind-body technique that involves using visual or auditory feedback to gain control over bodily functions. Normally, little voluntary control is needed to maintain continence, but surgical or other treatment can disrupt this balance.
The idea of biofeedback is to strengthen and gain more voluntary control of the urinary sphincter and pelvic floor muscles to increase continence. Biofeedback has been used to treat numerous physical and mental health issues, including incontinence. It can be used to complement and direct Kegal exercises.
A 2000 randomized trial directed at incontinence and published in the Lancet medical journal found that approximately 14 percent of participants using biofeedback achieved a greater degree of control over their incontinence than in the control group. [Van Kampen].
However, keep in mind that biofeedback involves retraining and gaining new control over muscles, and it might take a bit of time for positive effects to be noticed.
Non-Surgical Devices that May Help
While there are limited surgical options available, their effectiveness may vary. A recent Internet search yielded multiple products designed to help with male incontinence.
There are basically two groups of products; devices placed on the penis that compress the urethra and prevent undesired urine leakage, and absorbent products (pads, diapers) that absorb and retain the bladder leakage.
For many of these products not produced by their manufacturer, there may be limited independent information available. However, before considering a product, it would be wise to check the manufacturer’s website (if one exists) to see if a peer-to-peer interface is provided. Reviewing comments of other users can be very valuable for selecting a device that is acceptable.
Keep in mind that any device placed on the penis must be tight enough to hold the urethra closed and, thus, prevent leakage, yet not so tight as to prevent blood circulation. Generally, these devices are used for several hours at a time, and a diminishing of blood circulation to the penis for several hours can be disastrous.
Absorbent pads and underwear are another option. They are designed to absorb and retain fluid as well as keep liquid off the skin to avoid irritation. Depending on the degree of urge incontinence, success with them can vary considerably. Generally, very active men find them irritating and uncomfortable and usually opt for different control methods.
Condom Catheters
A condom catheter is a small device that affixes to the patient’s penis using a skin-friendly, temporary adhesive. The end opposite that attached to the penis is open and designed to accommodate a length of tubing. It is an inexpensive, disposable device that can be placed or removed at will.
A length of tubing can be attached to it and connected to a collection bag fastened to the patient′s leg or body to collect expelled urine. Unlike a regular Foley catheter, it does not contain the tubes or balloons passed through the penis and into the bladder.
A condom catheter can be worn at any time when leakage is expected. Since it is a temporary use device, it can be removed at any convenient time. Most men use one for temporary exertions during sports or for nighttime incontinence (see below).
Condom catheters can be obtained through a medical supply house. Some states may require a doctor′s prescription; others may not. In some cases, medical supply costs may be covered by relevant insurance or healthcare programs.
Nighttime Incontinence – Bedwetting
One of the most annoying consequences of incontinence is when it gets more severe at or during sleep. After surgery, some men find the can get by during the day using a pad or two, but the flow increases substantially while they are sleeping. This typically results in a “puddle” of urine accumulated during sleep that can be very disconcerting for the patient.
A condom catheter (as described above) can be a very useful solution for this problem. One end is fastened to the penis before sleep with the adhesive provided on the inside of the condom. The other end attaches to tubing connected to a standard urine collection bag. The collection bag can be attached to the patient’s leg or the bed with elastic straps. Urine released while sleeping is collected in the bag, which is then removed and cleaned in the morning for reuse.
Some condom catheters designed for nocturnal bedwetting may be intended for single-use, while others can be cleaned and reused as needed. Since these devices are rather inexpensive, several can be used daily as needs dictate. The collection bag can be cleaned and reused as often as needed.
Medical and Surgical Treatments for Incontinence
Artificial Urinary Sphincter
The current gold standard for the treatment of severe urinary incontinence after radical prostatectomy is the artificial urinary sphincter. The device consists of three parts that are embedded surgically; a urinary cuff, a small fluid storage balloon and a pump to move fluid from the balloon and back.
The urinary cuff is surgically placed around the urethra just below the urethral sphincter. When the cuff is closed, it acts as a natural urinary sphincter muscle and does not allow any urine to pass.
The pump is typically surgically placed in the scrotum. It is activated when necessary to urinate. Activation transfers fluid from the urinary cuff to the storage balloon. With the cuff empty, its pressure on the urethra is relaxed, and urine begins to flow out of the body.
The tension between the balloon and the cuff is usually set at the time of surgery so that the cuff refills and closes after about 3 minutes. Thus, when the patient activates the pump in the scrotum, urine begins to flow through the urethra until the urinary cuff refills fluid from the storage balloon. This ends the urine stream if it has not already stopped. If the patient feels his bladder has not been completely emptied, he simply repeats the process.
Implanting an artificial urinary sphincter is a minor surgery, but as such, it carries similar risks as other minor surgeries, including pain, bleeding, and infection at the insertion site.
In addition, a problem with any part of the device may necessitate surgery to remove or replace it. While these devices are typically very reliable, they do fail, and sometimes they may wear out over time and need to be replaced.
Various studies show that a high percentage of men using these devices (more than 90 percent) were satisfied with their performance. Some individuals experienced complications necessitating follow-up surgery within five years after the initial artificial urinary sphincter implantation.
Bulking Agents
In this procedure, a bulking agent, such as collagen, is injected into the tissue around the urethra. This causes a narrowing of the urethra so that it closes more readily. This procedure has not shown successful long-term results, although many men have found it a plausible short-term solution.
It is best viewed as a temporary measure or an option for men who cannot undergo invasive surgery. One of its disadvantages is that it can cause a urinary flow stoppage in some men if too much bulking agent is used or if the bulking agent migrates.
Sling Surgeries and Procedures
These procedures involve an incision between the scrotum and the rectum into which a supportive sling is installed under and around the urethra.
The principle is to place pressure on the urethra to help it remain closed and retain urine until the bladder fills. Typically, the sling is anchored to the pelvic bone on each side to maintain tension.
Several types of sling procedures exist, using different materials for the sling itself, but the efficacy of all of them is similar. This is a surgical procedure that involves a short hospital stay and has the same risks as other similar surgical procedures.
If a general anesthetic was used, patients would usually need to stay in the hospital for at least 3 to 4 hours after the procedure. If there are any problems passing urine after the procedure, an overnight hospital stay might be needed.
The recovery time for sling surgery varies, with most doctors recommending 2 to 4 weeks before returning to strenuous activities. It’s important to discuss the procedure’s risks and benefits with your healthcare provider.
Conclusion
Many urologists tend to minimize the effects of post-surgery incontinence. While it is not a medical problem that causes treatable disability or disease, it is, most certainly, a huge disruption of a man′s quality of life.
Male incontinence can be brought on by medical conditions like enlarged prostate, diabetes, and Parkinson’s disease, and other medical conditions. However, according to search engines, the most prevalent causes are side effects of medical procedures, especially radical prostatectomy.
No man wants to walk around wearing a diaper, but many men enter into medical treatment for prostate problems without careful consideration of the side effects of the treatment. In my practice, I have come across many men regretful of the medical treatment they received. A common theme for most of them is that the side effects are worse than the disease!
Explore More

New Study Investigates Treatment-Associated Regrets In Prostate Cancer.